People tend to assume that as dentists, we only care if our patients brush and floss their teeth regularly. While it’s true that we appreciate good at-home dental care, we know that oral health goes beyond brushing and flossing and can be impacted by activities like smoking and vaping.
For that reason, we’d like to discuss with you the harmful effects that electronic cigarettes have on oral health, despite their reputation as a safe alternative.
What is an E-Cigarette?
An e-cigarette refers to a handheld electronic device that creates an aerosol by heating a liquid, typically made of nicotine, propylene glycol, glycerine, and flavourings. E-cigarette users inhale this aerosol, which is called “vaping.”
Why do People Vape?
Many cigarette smokers use vaping as a method to quit smoking. Because e-cigarettes don’t have tobacco in them, vaping has long been thought of as a healthier alternative to smoking. However, studies are beginning to show that it’s not quite a harmless habit.
How Does Vaping Affect My Health?
Just as with smoking, vaping has negative health effects. Despite their lack of tobacco, e-cigarettes still contain nicotine, the highly addictive drug that is found in real cigarettes which causes a number of negative effects when ingested. In one study from the Journal of the Indian Society of Periodontology reported that nicotine may have a significant contribution to the development of both gingivitis and periodontitis. In addition, nicotine use can actually mask the bleeding gums side effect of gingivitis, making it more difficult to be diagnosed.
In one study of habitual e-cigarette users and non-users, e-cigarette users showed increased adrenaline in the heart, and greater oxidative stress; two factors that increase the risk of cardiovascular disease, including heart attacks, gum disease and strokes. Unfortunately, your heart is not all vaping can harm.
Because the mouth is the first place the vapor goes, it’s also when it’s the most concentrated, and hot. A popular complaint about side effects from using e-cigarettes is “mouth and throat dryness and irritation.” In a separate study, researchers placed mouth cells in a chamber before pumping in e-cigarette vapor to monitor the effects. After just three days, 53% of the mouth cells were dead or dying. By comparison, mouth cells that weren’t exposed to the e-cigarette vapor only had a 2% death rate.
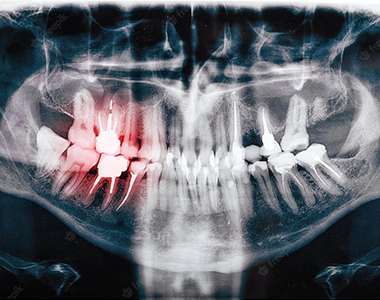
Users have also experienced the extreme danger involved with e-cigarettes overcharging and exploding. Multiple incidents have been reported where e-cigarettes explode while being used , knocking out teeth and damaging tongue, cheeks and lips. Hence requiring extensive dental, cosmetic and surgical repair to restore their once beautiful smile.
How Does Vaping Compare to Smoking?
Because e-cigarettes haven’t been around as long as regular cigarettes, we don’t have long-term research comparing the two. However, in a recent study done by Cancer Research UK-funded scientists, people who swapped cigarettes for e-cigarettes or nicotine replacement therapy had significantly lower levels of toxic chemicals and carcinogens in their bodies.
Many choose to believe that means e-cigarettes are a safe alternative, but that’s not the case. It merely means that potentially, they are less damaging than real cigarettes. However, more research is required before that can be said conclusively.
What About Using E-Cigarettes to Quit Smoking?
It’s all too common for people to replace an addiction with another one. This is true for cigarette addictions as well, many people end up with an e-cigarette addiction as a result. Our professional recommendation is to avoid vaping altogether, as it causes damage to not only your oral health but your overall well-being.
Speaking of cigarettes, it’s very important for smokers to visit their dentist regularly so their oral health can be monitored. Our goal is your complete health, and the end goal with smoking is to quit.


 Review Us
Review Us Review Us
Review Us